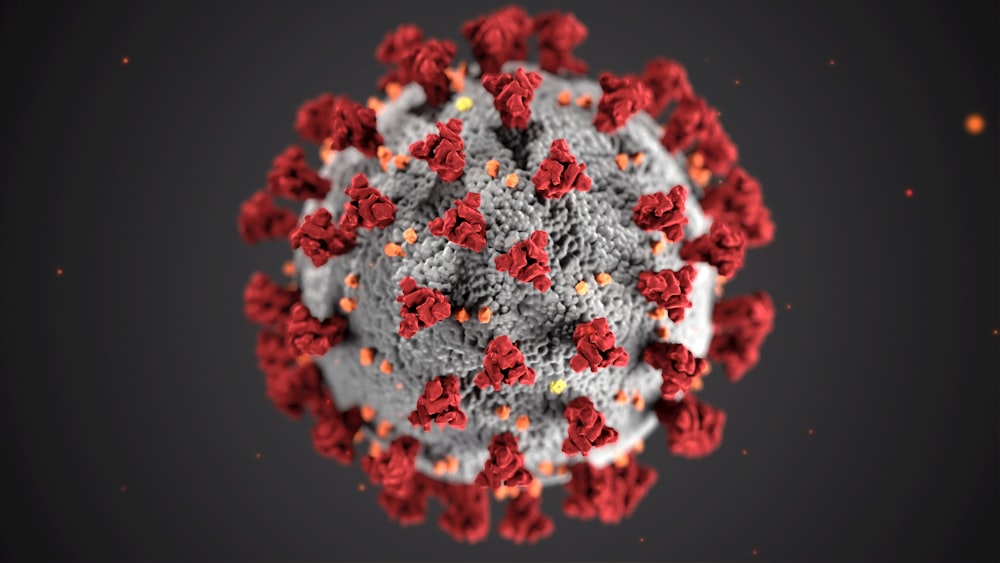
Coronavirus
How COVID-19 is changing services for Medicare Beneficiaries. For more info on Medicare your health and the Corona Virus(COVID-19) check out our last blog. Because of COVID-19, Social distancing has been put into place. That is changing things for Medicare beneficiaries. Services that were presented person to person are being reduced and services by phone or device are on the rise. The COVID-19 is changing how Medicare beneficiaries receive services.
As of 3/6/2020 Medicare will pay for telehealth services for patients. This includes doctors, hospital, clinics, skilled nursing, or community mental health clinics. You can now be seen by any of those by phone or device and have medicare pay it’s portion. Medicare Advantage plans from United Healthcare, Humana, Centene, or Aetna can cover even more benefits. Call us and we can help you know what benefits are covered by your plan.
The reasons that they have introduced these changes is COVID-19 has a 5-14 days period in which you are spreading the virus before you start to feel its effects. So someone can have and pass on the virus and feel completely healthy. There is also a problem with testing, many doctors offices, clinics or hospitals cannot keep up with demand for the tests needed.
According to the World Health Organization (WHO) the risk of catching COVID-19 is still low. Follow the info from reputable sites like the CDC or WHO
What things should I do to avoid COVID-19
- Regularly clean hands with soap and water.
- Maintain a distance of at least 3 ft with someone who is coughing or sneezing.
- Avoid touching mouth, eyes or nose.
Hand washing is important to remain healthy.
- cover mouth and nose with facial tissue or elbow if coughing or sneezing.
- Stay home when possible.
- Reduce travel.
The following measures ARE NOT effective against COVID-2019 and can be harmful:
- Smoking
- Wearing multiple masks
- Taking antibiotics
Check out our website for more medicare info
We also have a Youtube channel
Like us on Facebook








